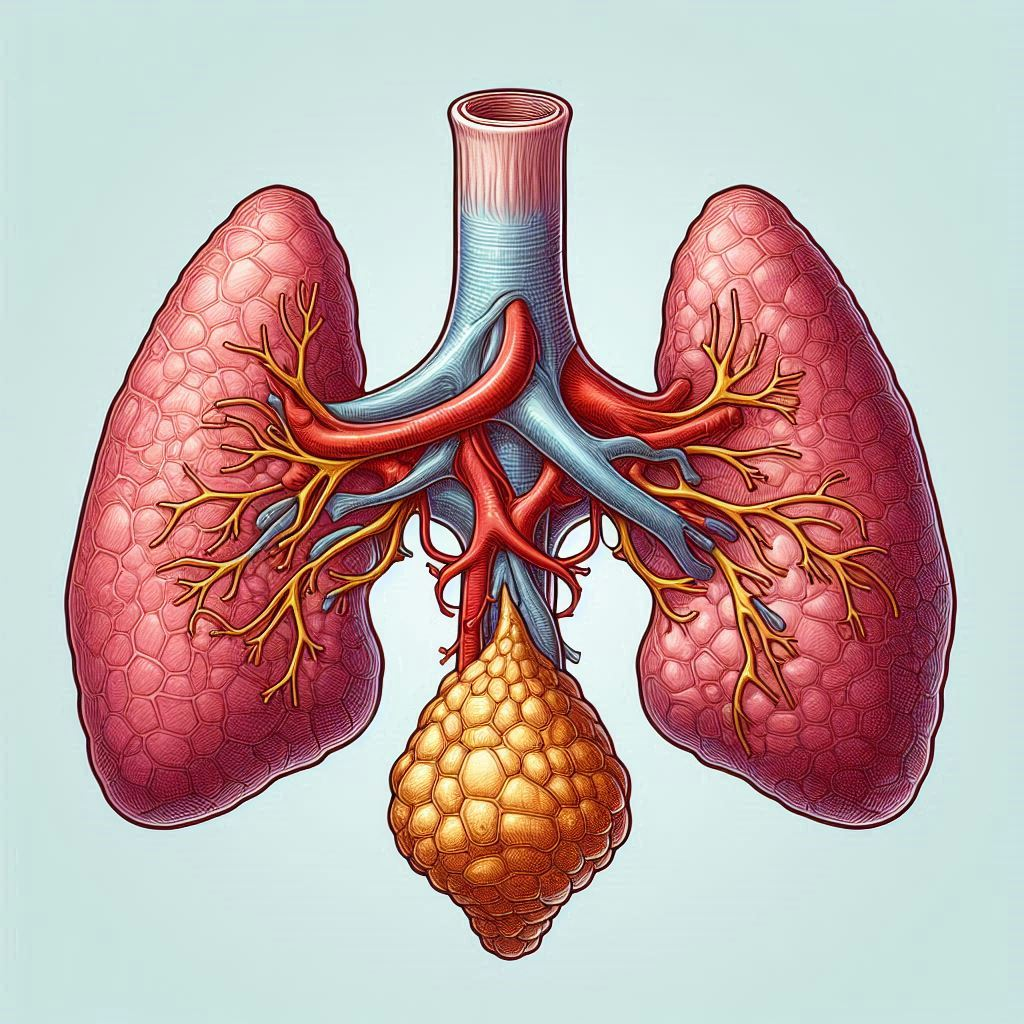
What is thymus gland?
The thymus gland is a specialized organ of the immune system situated in the upper chest, directly behind the sternum (breastbone) and in front of the heart.
It is essential for the immune system’s growth and operation, especially in the early stages of life.
Anatomy
Location: The thymus gland is located above the superior vena cava, in front of the heart, and behind the sternum, or breastbone. Its length varies during life as it extends upward to the base of the neck.
Structure: The thymus gland is composed of two lobes that are connected by a central isthmus. Each lobe is further subdivided into smaller lobules.

Blood Supply: The internal thoracic arteries and veins branch off to supply to the thymus gland with blood.
Histological Structure: The thymus is divided into two distinct regions within each lobule-
Cortex: Thymocytes, or immature T-cells, are closely packed and undergoing maturation and selection processes in the outer portion of each lobule.
Medulla: The inner area is home to better developed thymocytes as well as dendritic and epithelial cells that are involved in T-cell selection and education.
Developmental Changes: The thymus gland gradually involutes (shrines and becomes less active) with age, peaking in activity and size throughout infancy and youth. Its functional capacity decreases with age and it has more fatty tissue.
Functions of thymus
The thymus gland plays several critical roles in the body’s immune system, particularly during early life and development. Here are the key roles of the thymus:
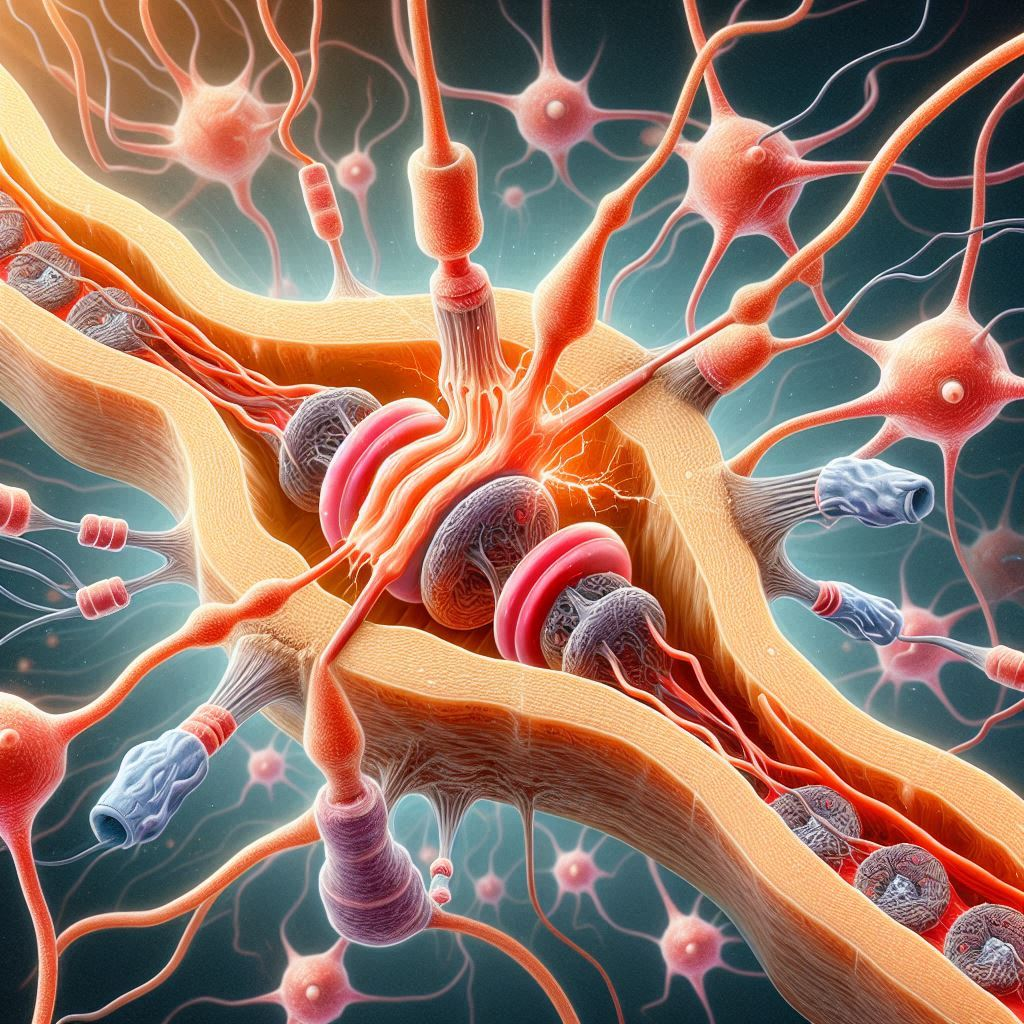
Maturation of T-cells: Derived from bone marrow, immature T-cells travel to the thymus where they go through a maturation and training process. The thymus’s main job is to support the maturation and differentiation of T-lymphocytes (T-cells), a type of white blood cell essential for adaptive immunity.
T-cell Selection: In the thymus, developing T-cells are exposed to self-antigens—molecules that have the potential to elicit an immune response—displayed by specialized cells, including thymic epithelial cells and dendritic cells. Central tolerance is the process by which the T-cells learn to discriminate between self and non-self antigens. This exposure facilitates this process. Negative selection results in the elimination of T-cells that bind and identify strongly to self-antigens, limiting autoimmune reactions in which the body’s own tissues are attacked by the immune system.
Diversity of T-cell Generation: The thymus plays a role in the T-cell receptor repertoire’s diversity, which enables the immune system to identify and react to a variety of pathogens.
Production of Hormones: The thymus gland secretes a number of hormones, including thymosin, which is involved in the T-cells’ maturation and differentiation.

Immune System Education: The thymus instructs the immune system so that it can respond to infections efficiently and prevent damaging immunological reactions against the body’s own tissues through the processes of T-cell maturation and selection.
Early Life Immune Defense: The thymus is extremely active throughout fetal development and the first few months of infancy, and it is essential for building the immune system’s capacity to fight infections.
Role in Autoimmunity and Immunodeficiency: Immune illnesses, such as autoimmune diseases (in which the immune system unintentionally assaults the body’s own tissues) and immunodeficiencies (in which the immune system is compromised), can result from thymus dysfunctions or abnormalities.
Functions of immune system
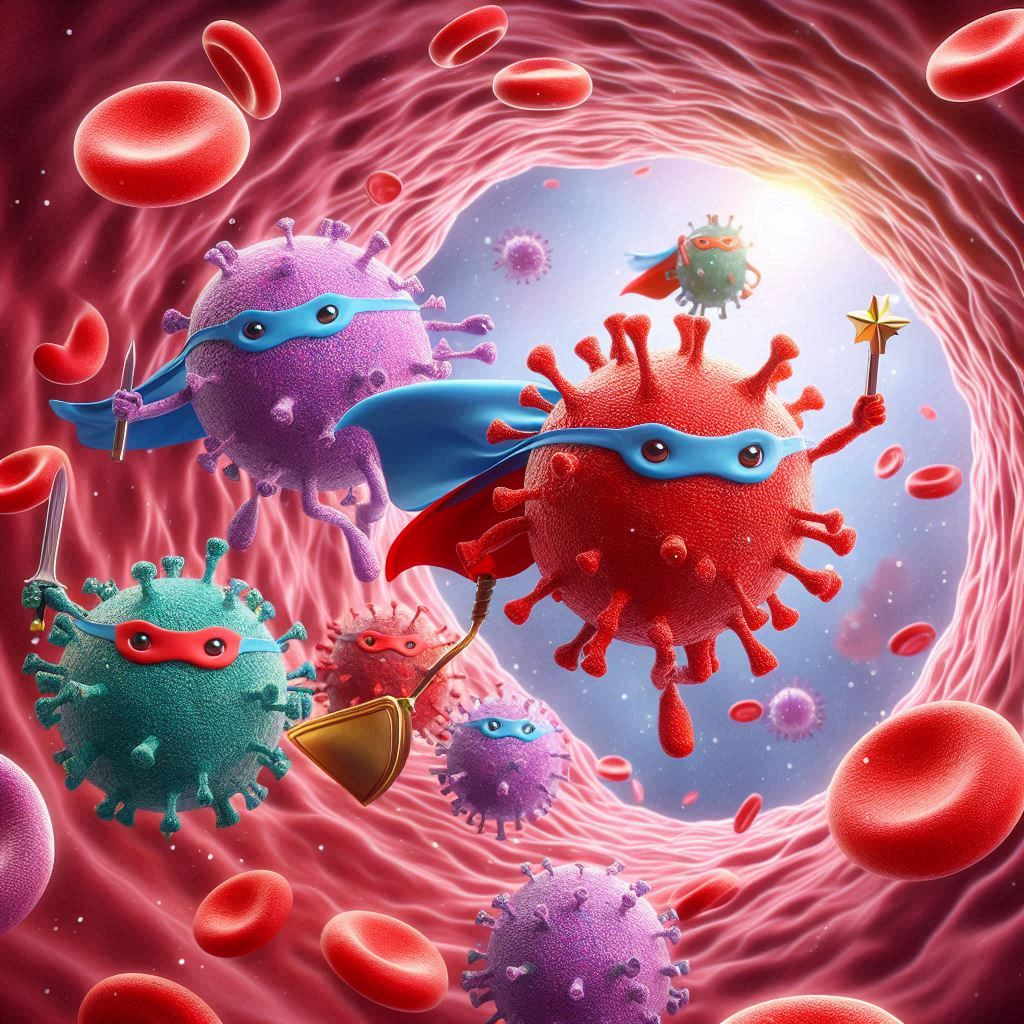
Identification and Response to Pathogens: Due to certain receptors on immune cells, the immune system can identify a large range of pathogens. These receptors have the ability to recognize chemicals (antigens) specific to infections, hence inducing an immune response.
Immune surveillance: Immune cells search the body continuously for indications of infection or abnormal cell proliferation. Any cells or molecules that are not a part of the body’s own healthy tissues are recognized by them, and they react accordingly.

Immune Response Activation: The immune system launches a systematic defense in response to the presence of a pathogen or foreign material. Immune cells, including T-cells, B-cells, and phagocytes (like macrophages), are activated and proliferate in this process in order to eradicate the intruder.
Production of Antibodies: Antibodies are specialized proteins produced by B-cells that attach to particular antigens on infections. Antibodies have the ability to immediately kill pathogens, label them for eradication by other immune cells, or initiate alternative immunological reactions.
Cellular Immunity: T-cells are essential to the process of cellular immunity. They have the ability to eliminate abnormal or infected cells directly, and they also aid in controlling the immune response by releasing cytokines, which are signaling chemicals that stimulate other immune cells.
Memory and Long-Term Defense: Certain immune cells develop memory cells following their first infection. Long-term immunity is provided by these cells, which “remember” the pathogen and can mount a quicker and more potent defense upon a later exposure.
Tolerance to Self: To prevent harming the body’s own healthy tissues, the immune system needs to be able to discriminate between self and non-self. This is accomplished by mechanisms such as peripheral tolerance (mediated by regulatory T-cells and other mechanisms) and central tolerance (in the thymus for T-cells).

Inflammation and Healing: An essential part of the immune response, inflammation serves to limit and destroy infections. In the event of an infection or damage, it also aids in the start of tissue repair and healing processes.
Relationships with Other Systems: The neurological, endocrine, and cardiovascular systems are just a few of the physiological systems with which the immune system interacts. These exchanges support immune response coordination and general health maintenance.
Immune Regulation: To avoid excessive inflammation or autoimmune diseases, the immune system uses a variety of mechanisms to control the length and severity of immune responses.
Disorders
Thymoma: Thymomas are tumors that start in the thymus gland’s epithelial cells. They may be malignant, or cancerous, or benign, or neither. Because of their size and position in the mediastinum, thymomas can induce symptoms in addition to disrupting normal thymus function (chest cavity).
Thymic hyperplasia: This disorder is characterized by an increase in thymic tissue as a result of thymus gland hypertrophy. It can happen as a result of a number of things, such as infections, autoimmune conditions (such myasthenia gravis), or a normal developmental stage in youngsters.
Myasthenia Gravis: This autoimmune disease, which frequently affects the voluntary muscles regulated by the nerves, is typified by weariness and muscle weakness. It is frequently linked to autoantibodies that attack muscle cell acetylcholine receptors. Myasthenia gravis patients have thymic abnormalities, such as thymoma or thymic hyperplasia, in a notable percentage of cases.
DiGeorge Syndrome: A little portion of chromosome 22 is missing, resulting in DiGeorge syndrome, also known as 22q11.2 deletion syndrome. Many symptoms may arise from it, such as underdeveloped or absent thymus glands, congenital cardiac problems, developmental delays, and irregularities in the immune system.

Thymic Aplasia or Hypoplasia: A person may have thymic aplasia or hypoplasia, which is the underdevelopment or absence of the thymus gland at birth. Those who have this illness may experience severe immunological deficits, which increases their sensitivity to infections.
Thymic Cysts: Within the thymus gland, thymic cysts are sacs filled with fluid. Generally benign, their size and placement determine whether they cause symptoms or are asymptomatic.
Thymic Carcinoma: Thymic carcinoma is a rare form of cancer that starts in the epithelial cells of the thymus gland. It can spread to other bodily areas and is more aggressive than thymoma.
Clinical Implications
Given its critical role in immune function, disruptions in thymus gland development or function can have significant clinical implications.

Immunodeficiency Disorders: Immunodeficiency disorders, which are characterized by decreased immune responses and more prone to infections, can result from disorders affecting thymus function, such as DiGeorge syndrome or thymic involution with aging. In extreme situations, management may include hematopoietic stem cell transplantation or immunoglobulin replacement therapy.
Autoimmune illnesses: Thymic dysfunction disorders like myasthenia gravis or autoimmune polyendocrine syndrome type 1 (APS-1) can lead to autoimmune illnesses, which are conditions in which the body’s own tissues are attacked by the immune system. In order to control symptoms and reduce immune-mediated harm, treatment approaches frequently center on immunosuppression or targeted immunomodulatory medications.
Thymectomy: To cure disorders like thymomas or myasthenia gravis, a thymectomy, or surgical removal of the thymus gland, may be required in certain circumstances. Depending on the underlying ailment and the patient’s state of health, a thymectomy may be performed to improve symptoms, lessen the size of the tumor, or control autoimmune reactions.

FAQ (frequently asked questions)
1. What is the thymus gland and where is it located?
- The thymus gland is a specialized organ of the immune system located in the upper part of the chest, behind the sternum (breastbone) and in front of the heart. It is part of the lymphatic system.
2. What is the function of the thymus gland?
- The thymus gland plays a crucial role in the development and maturation of T-lymphocytes (T-cells), a type of white blood cell important for immune function. It helps educate T-cells to distinguish between self and non-self antigens, thereby preventing autoimmune reactions.
3. How does the thymus gland contribute to immune function?
- The thymus gland produces and secretes hormones, such as thymosin, that support the maturation of T-cells. It provides an environment where immature T-cells develop into mature T-cells capable of recognizing and responding to pathogens.
4. When does the thymus gland function most actively?
- The thymus gland is most active during infancy and childhood, gradually becoming less active with age. It reaches its maximum size and function during early childhood and starts to involute (shrink) during puberty.
5. What are some disorders associated with the thymus gland?
- Disorders involving the thymus gland include thymomas (tumors), thymic hyperplasia (enlargement), myasthenia gravis (an autoimmune disorder), thymic aplasia or hypoplasia (underdevelopment or absence), and thymic cysts. These conditions can affect immune function and overall health.
6. How is a thymoma diagnosed?
- Thymomas are often discovered incidentally on imaging studies such as chest X-rays or CT scans. Diagnosis may involve biopsy for histological examination to determine the type of tumor and its potential impact on surrounding tissues.
7. What role does the thymus gland play in autoimmune diseases?
- The thymus gland is involved in educating T-cells to recognize and tolerate self-antigens. Dysfunctions in thymus function or development can lead to autoimmune diseases where the immune system mistakenly attacks the body’s own tissues, such as in myasthenia gravis.
8. Can disorders of the thymus gland be treated?
- Treatment for thymus gland disorders depends on the specific condition and its severity. Options may include medications, surgery to remove tumors or cysts, immunosuppressive therapy for autoimmune diseases, or supportive care to manage symptoms and complications.
9. Is removal of the thymus gland (thymectomy) necessary in certain conditions?
- Thymectomy may be performed in cases of thymoma, myasthenia gravis, or other thymus-related disorders where surgical removal of the gland is indicated to alleviate symptoms or prevent complications.
10. How does aging affect the thymus gland?
- With aging, the thymus gland undergoes involution (shrinkage) and becomes less active. This age-related change is associated with decreased production of new T-cells, contributing to age-related decline in immune function known as immunosenescence.
Conclusion
The thymus gland stands as a remarkable example of nature’s elegant design, orchestrating the education and deployment of T-cells that are essential for our immune defenses. From its pivotal role in shaping adaptive immunity to its susceptibility to disorders impacting immune function, the thymus remains a focal point of scientific inquiry and clinical relevance. As our understanding of thymic biology continues to evolve, so too does our ability to harness its potential for improving human health and combating disease.
Table of Contents
Read more about Thymus gland
Restriction endonucleases-applications, challenges…
Go and visit dusearchit.in and get more knowledge about others topics.
