What is pancreas?
Pancreas is a mixed gland which acts as a endocrine and exocrine gland.
It is a vital organ located behind the stomach and is an essential part of the digestive and endocrine systems in the human body.
Anatomy
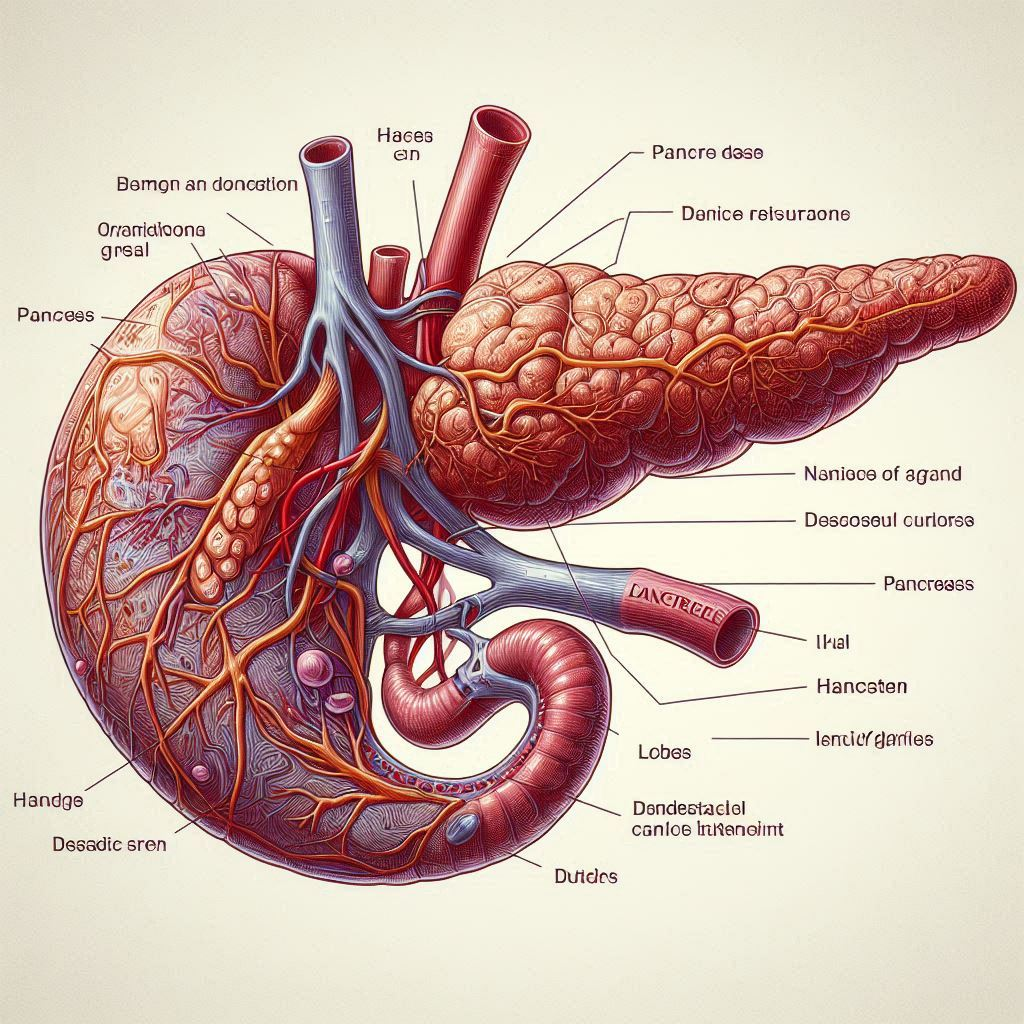
The pancreas is a glandular organ located in the abdomen, positioned behind the stomach and next to the duodenum, which is the first part of the small intestine.
The pancreas is roughly triangular in shape and has a head, a body, and a tail:
Head: The head of the pancreas is the widest part and is nestled within the curve of the duodenum.
Body: The body of the pancreas extends horizontally across the abdomen behind the stomach.
Tail: The tail of the pancreas tapers off to the left side of the abdomen near the spleen.
Blood Supply: The pancreas receives its blood supply from branches of the splenic artery, superior mesenteric artery, and gastroduodenal artery.
Nerve Supply: Nerve fibers from the autonomic nervous system (sympathetic and parasympathetic nerves) control pancreatic functions, including secretion of enzymes and hormones.
The pancreas has a complex duct system that transports digestive enzymes produced by pancreatic acinar cells to the duodenum. The main pancreatic duct joins with the common bile duct near the duodenum, forming the hepatopancreatic ampulla (ampulla of Vater), which releases its contents into the duodenum through the major duodenal papilla.
Histology
Exocrine Portion-
Acinar Cells:
- Acinar cells are the predominant cells in the exocrine portion of the pancreas.
- They form clusters called acini, which are small sac-like structures.
- Acinar cells secrete digestive enzymes into small ducts that eventually merge into larger pancreatic ducts.
Endocrine Portion-
Islets of Langerhans:

- These are spherical clusters of endocrine cells scattered throughout the pancreas.
- Islets of Langerhans contain different types of cells, including:
- Beta Cells: Secrete insulin, which helps lower blood glucose levels.
- Alpha Cells: Secrete glucagon, which increases blood glucose levels.
- Delta Cells: Secrete somatostatin, which inhibits the secretion of insulin and glucagon.
- PP Cells (Pancreatic Polypeptide Cells): Secrete pancreatic polypeptide, which regulates pancreatic exocrine function and appetite.
Functions
The pancreas serves crucial functions in both the digestive and endocrine systems of the human body. Here are the main functions of the pancreas:
Exocrine Functions-
1. Production of Digestive Enzymes:

Amylase: Produces sugars like glucose and maltose from the breakdown of carbohydrates (starch).
Lipase: Converts fats (lipids) into glycerol and fatty acids.
Proteases: Reduce proteins to smaller peptides and amino acids (e.g., trypsin, chymotrypsin).
2. Regulation of Digestive Juice Composition:
In order to counteract the acidic chyme, or partially digested food, coming from the stomach, the pancreas also secretes bicarbonate ions. In the small intestine, this produces the ideal pH environment for the activity of digesting enzymes.
Endocrine Functions-
1. Regulation of Blood Glucose Levels:
Insulin: When blood glucose levels are high, beta cells release the hormone insulin. Insulin lowers blood glucose levels by facilitating glucose absorption into cells.
Glucagon: Alpha cells release glucagon when blood glucose levels are low. Blood glucose levels rise as glucagon encourages the liver to release stored glucose into the bloodstream.

2. Other Hormones:
Somatostatin: Secreted by delta cells, somatostatin inhibits the release of insulin and glucagon, helping to regulate their balance. Pancreatic Polypeptide (PP): Secreted by PP cells, pancreatic polypeptide helps regulate pancreatic secretion activities and food intake.
Additional Functions-
1. Digestive Enzyme Activation: The pancreas also plays a role in activating digestive enzymes that are secreted in an inactive form (zymogens). For example, trypsinogen is converted to trypsin, which then activates other pancreatic enzymes.
2. Fluid and Electrolyte Balance: The secretion of pancreatic juices containing enzymes and bicarbonate ions helps maintain fluid and electrolyte balance in the digestive tract.
Disorders
Disorders of the pancreas can significantly impact both its exocrine (digestive enzyme production) and endocrine (hormone production) functions. Here are some common disorders associated with the pancreas:
Exocrine Pancreatic Disorders-
1. Pancreatitis:

- Acute Pancreatitis: Sudden inflammation of the pancreas, often due to gallstones or excessive alcohol consumption. Symptoms include severe abdominal pain, nausea, vomiting, and fever.
- Chronic Pancreatitis: Persistent inflammation and scarring of the pancreas, typically due to long-term alcohol abuse or certain genetic conditions. Symptoms include recurring abdominal pain, malabsorption, weight loss, and diabetes mellitus.
2. Pancreatic Cancer:
Pancreatic cancer is a malignant tumor that develops in the tissues of the pancreas. It is often diagnosed at an advanced stage due to nonspecific symptoms such as abdominal pain, weight loss, jaundice (yellowing of the skin and eyes), and digestive issues.
3. Pancreatic Insufficiency:
This condition occurs when the pancreas does not produce enough digestive enzymes (e.g., due to chronic pancreatitis or cystic fibrosis). It leads to malabsorption of nutrients, causing symptoms like diarrhea, steatorrhea (fatty stools), weight loss, and nutritional deficiencies.
Endocrine Pancreatic Disorders-
1. Diabetes Mellitus:

Type 1 Diabetes: Results from autoimmune destruction of insulin-producing beta cells in the pancreas, leading to insulin deficiency. Requires lifelong insulin therapy for blood sugar control. Type 2 Diabetes: Develops due to insulin resistance and eventual beta cell dysfunction. Managed initially with lifestyle changes and medications, but may progress to requiring insulin therapy.
2. Pancreatic Endocrine Tumors (Pancreatic Neuroendocrine Tumors, PNETs):
These are rare tumors that arise from the endocrine cells of the pancreas (islet cells). They can be functional (secreting hormones like insulin, glucagon, etc.) or non-functional (not secreting hormones). Symptoms depend on hormone secretion and tumor size/location.
Other Disorders-
Pancreatic Cysts:
- Fluid-filled sacs within the pancreas, which can be benign or malignant. Often incidental findings on imaging studies and may require monitoring or intervention depending on size and symptoms.

Pancreatic Stones:
- Calcifications within the pancreatic ducts, which can obstruct the flow of digestive enzymes and bile. Associated with chronic pancreatitis and may cause recurrent abdominal pain and complications.
Diagnosis
1. Clinical Evaluation–
- Medical History and Physical Examination: The doctor will ask about symptoms such as abdominal pain, nausea, vomiting, weight loss, changes in bowel habits, and jaundice (yellowing of the skin and eyes). A thorough physical examination may reveal abdominal tenderness, palpable masses, or signs of malnutrition.
2. Laboratory Tests–

- Blood Tests:
- Amylase and Lipase: Elevated levels of these enzymes in the blood suggest acute pancreatitis.
- Glucose: Elevated blood glucose levels may indicate pancreatic endocrine disorders such as diabetes mellitus.
- CA 19-9 and CEA: Tumor markers that may be elevated in pancreatic cancer.
3. Imaging Studies–
- Ultrasound: Provides initial evaluation, especially for gallstones and pancreatitis. It can also visualize pancreatic tumors and cysts.
- Computed Tomography (CT) Scan: Offers detailed images of the pancreas and surrounding structures, helpful for detecting tumors, pancreatitis, and pancreatic duct abnormalities.
- Magnetic Resonance Imaging (MRI): Particularly useful for pancreatic tumors, cysts, and evaluating pancreatic ducts. MRI with MRCP (Magnetic Resonance Cholangiopancreatography) is used to assess the pancreatic duct system.
- Endoscopic Ultrasound (EUS): Combines endoscopy with ultrasound to obtain detailed images of the pancreas and nearby structures, useful for detecting tumors and obtaining biopsies.

4. Endoscopic Retrograde Cholangiopancreatography (ERCP)–
- An invasive procedure where a flexible tube (endoscope) is passed through the mouth and into the duodenum to inject contrast dye into the pancreatic and bile ducts. It helps visualize ductal anatomy and detect blockages or structural abnormalities.
5. Biopsy and Pathological Examination–
- Fine Needle Aspiration (FNA): A biopsy procedure where a thin needle is inserted into the pancreas under guidance (usually CT or EUS) to obtain tissue samples for pathological examination. Helps diagnose pancreatic tumors and assess their type and stage.

FAQ (frequently asked questions)
1. What is the pancreas and where is it located? Ans. The pancreas is a glandular organ located in the abdomen, behind the stomach and next to the duodenum (the first part of the small intestine).
2. What are the functions of the pancreas? Ans. The pancreas has two main functions:
- Exocrine Function: It produces digestive enzymes (such as amylase, lipase, and proteases) that help break down carbohydrates, fats, and proteins in the small intestine.
- Endocrine Function: It produces hormones (such as insulin and glucagon) that regulate blood sugar levels.
3. What is pancreatitis? Ans. Pancreatitis is inflammation of the pancreas. It can be acute (sudden onset, often due to gallstones or excessive alcohol consumption) or chronic (persistent inflammation and damage, often due to long-term alcohol abuse or other factors).
4. What are the symptoms of pancreatitis? Ans. Symptoms of pancreatitis may include severe abdominal pain (often radiating to the back), nausea, vomiting, fever, rapid pulse, and in severe cases, shock.
5. What is diabetes mellitus and how is it related to the pancreas? Ans. Diabetes mellitus is a metabolic disorder characterized by high blood sugar levels over a prolonged period. It occurs due to either insufficient insulin production (Type 1 diabetes) or the body’s ineffective use of insulin (Type 2 diabetes), both of which involve dysfunction of the pancreas.
6. What is pancreatic cancer? Ans. Pancreatic cancer is a malignant tumor that develops in the tissues of the pancreas. It is often diagnosed at an advanced stage due to nonspecific symptoms such as abdominal pain, weight loss, jaundice, and digestive issues.
7. How is pancreatic cancer diagnosed? Ans. Diagnosis of pancreatic cancer typically involves imaging tests such as CT scan, MRI, and endoscopic ultrasound (EUS), as well as biopsy to confirm the presence of cancerous cells.
8. Can pancreas disorders be prevented? Ans. Some pancreas disorders, such as acute pancreatitis due to gallstones or excessive alcohol consumption, may be preventable by avoiding risk factors. Maintaining a healthy lifestyle, including a balanced diet and regular exercise, may also help reduce the risk of developing diabetes mellitus or pancreatic cancer.
9. What is the treatment for pancreatitis? Ans. Treatment for pancreatitis depends on the severity and cause. It may include fasting (to rest the pancreas), intravenous fluids, pain management, and in severe cases, surgery to remove damaged tissue or treat complications like infected pancreatic necrosis.
10. How does the pancreas affect digestion? Ans. The pancreas secretes digestive enzymes into the small intestine to break down carbohydrates, fats, and proteins into smaller molecules that can be absorbed by the body. Without sufficient pancreatic enzyme production (as seen in pancreatic insufficiency), digestion and nutrient absorption can be impaired.
Conclusion
The pancreas is an indispensable organ with dual functions critical to digestion and metabolic regulation. Its intricate structure and hormone-secreting capabilities underscore its significance in maintaining overall health. Understanding its anatomy, functions, and the impact of pancreatic disorders is crucial for early detection, effective treatment, and ongoing research to enhance our knowledge and therapies related to this vital organ. As research continues to evolve, so too will our ability to combat diseases of the pancreas and improve patient outcomes worldwide.
Table of Contents
Read more about Pancreas
Thymus gland-anatomy, hormones, disorders....
Go and visit dusearchit.in and get more knowledge about others topics.

Pingback: Adrenal gland- functions, hormones, disorder..(2024)
Your site visitors, especially me appreciate the time and effort you have spent to put this information together. Here is my website UQ8 for something more enlightening posts about Thai-Massage.
thanks alot!! and check my other blogs also
Hey there, I appreciate you posting great content covering that topic with full attention to details and providing updated data. I believe it is my turn to give back, check out my website 63U for additional resources about Cosmetic Treatment.