What is Malaria?
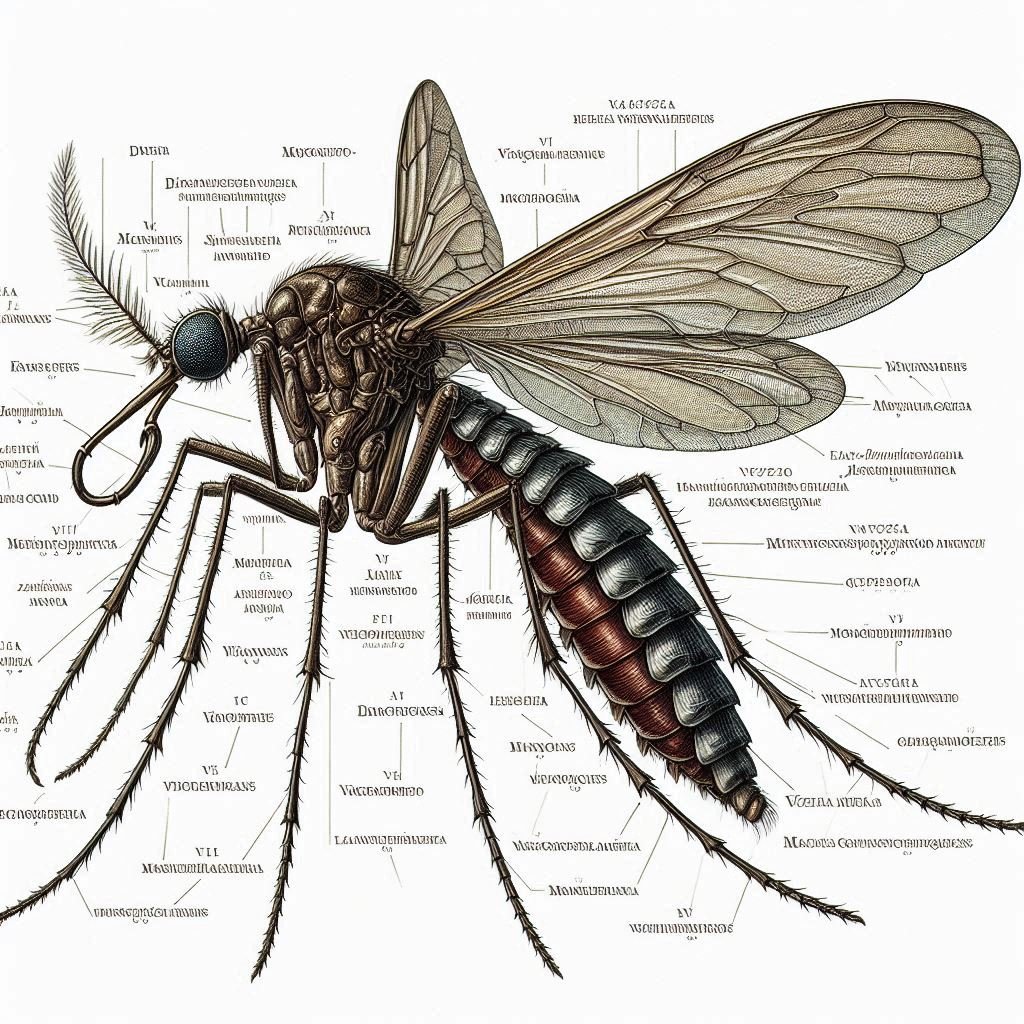
Malaria is a potentially deadly disease caused by a protozoan known as Plasmodium genus. When infected female Anopheles mosquitoes bite humans to feed on blood, they can transmit these parasites into the human bloodstream. Once inside the body, the parasites travel to the liver, where they mature and reproduce.
Global impact
Globally, an approximately 2.1 billion malaria cases and 11.7 million malaria deaths were recorded in the 2000-2022 period.
Types of malaria
The most common types of malaria include:
Plasmodium falciparum: This is most serious and responsible for the majority of malaria-related deaths globally. It is prevalent in sub-Saharan Africa but can also be found in other parts of the world. Plasmodium falciparum can progress rapidly to severe illness and complications if left untreated.

Plasmodium vivax: This species is widespread in many parts of the world, including Asia, Latin America, and parts of Africa. Plasmodium vivax can cause recurrent episodes of illness because it can remain dormant in the liver and reactivate months or even years later.
Plasmodium malariae: This species is less common but can cause a chronic and long-lasting form of malaria. Plasmodium malariae is found in various regions of Africa, Asia, and South America.
Plasmodium ovale: Plasmodium ovale is relatively rare compared to other types but is found in parts of Africa, Southeast Asia, and the Pacific islands. It can cause recurrent episodes of illness similar to Plasmodium vivax .
Plasmodium knowlesi: This species primarily infects monkeys but can also infect humans. Plasmodium knowlesi is found in parts of Southeast Asia and has become a concern in regions where deforestation and human activities bring humans into closer contact with macaque monkeys.
How Plasmodium enters into our body?
Plasmodium, the parasite responsible for malaria, enters the human body through the bite of an infected female Anopheles mosquito in a form of sporozoites (infectious form).

Parasite get into liver and multiply in liver cell and then attacks the red blood cell(RBC) and result in their rupture and because of rupturing the RBC it releases a toxic substance called Haemozoin and it is responsible for the chills and high fever in every 3-4 days.
When female anopheles mosquito bites infected person with malaria then the parasites enter into mosquito body and the parasites gets multiply to form sporozoites and these gets stored in their salivary gland.
And again when these mosquito bite a person the sporozoites introduced in their body and it forms a complete cycle.
Note : for completing the life cycle malarial parasites requires 2 hosts- Human and mosquito.
Symptoms
The symptoms of malaria can vary depending on factors such as the species of Plasmodium causing the infection, the individual’s immunity, and the severity of the illness. However, common symptoms include:
1.Fever: Fever is one of the hallmark symptoms of malaria. It can be intermittent, with spikes in temperature occurring every few days, depending on the type of Plasmodium causing the infection.

2.Chills: Chills often accompany the fever and may be severe, leading to shaking or shivering.
3.Sweating: Profuse sweating can occur as the fever breaks during the course of the illness.
4.Headache: Headaches are common and can range from mild to severe.
5.Muscle aches: Generalized muscle aches and body pains are frequently reported by individuals with malaria.
6.Fatigue: Malaria can cause extreme fatigue and weakness, leading to decreased energy levels and activity.
7.Nausea and vomiting: Some individuals with malaria may experience nausea and vomiting, especially during the early stages of the illness.

8.Loss of appetite: Loss of appetite is common and may contribute to weight loss and nutritional deficiencies.
9.Abdominal pain: Abdominal pain and discomfort can occur, often accompanied by diarrhea.
10.Jaundice: In severe cases of malaria, particularly those caused by Plasmodium falciparum, jaundice (yellowing of the skin and eyes) may develop due to liver dysfunction.
Preventions
Use of Insecticide-Treated Bed Nets (ITNs): Sleeping under ITNs helps protect individuals from mosquito bites during the night when Anopheles mosquitoes, which transmit malaria, are most active. ITNs are particularly effective for vulnerable populations such as children and pregnant women.
Indoor Residual Spraying (IRS): IRS involves spraying insecticides on the interior walls of houses and other structures to kill mosquitoes that land on them. This helps reduce mosquito populations and malaria transmission indoors.

Mosquito Control: Eliminating mosquito breeding sites by draining stagnant water, covering water storage containers, and using larvicides can help reduce mosquito populations and prevent malaria transmission.
Personal Protection Measures: Wearing long-sleeved clothing, using insect repellents on exposed skin, and avoiding outdoor activities during peak mosquito activity times (dusk and dawn) can help reduce the risk of mosquito bites.
Chemoprophylaxis: Travelers to malaria-endemic areas may be prescribed antimalarial drugs for preventive use. These drugs help prevent malaria infection but must be taken according to a healthcare provider’s recommendations and continued after leaving the malaria-endemic area, depending on the specific medication.
Intermittent Preventive Treatment in Pregnancy (IPTp): Pregnant women in malaria-endemic areas may receive preventive treatment with antimalarial drugs to protect themselves and their unborn babies from malaria infection.
Community Education: Providing information to communities about malaria transmission, prevention methods, and the importance of seeking prompt medical care for suspected cases can empower individuals to protect themselves and their families from malaria.
Prompt Diagnosis and Treatment: Early diagnosis and treatment of malaria cases are essential for preventing severe illness, complications, and onward transmission of the disease. Access to effective antimalarial drugs and healthcare services is crucial for successful malaria control.
Treatment
Artemisinin-based Combination Therapies (ACTs): ACTs are the recommended first-line treatment for uncomplicated malaria caused by Plasmodium falciparum, the most deadly species of malaria parasite. These combinations typically include an artemisinin derivative (such as artemether or artesunate) combined with another antimalarial drug (such as lumefantrine, mefloquine, or piperaquine). ACTs are highly effective at rapidly reducing the parasite load in the body.

Chloroquine: Chloroquine was historically the first-line treatment for malaria in many parts of the world, but due to widespread resistance, its use has been limited. However, in areas where Plasmodium vivax or Plasmodium ovale malaria remains sensitive to chloroquine, it may still be used for treatment.
Quinine and Quinidine: Quinine and its derivative, quinidine, are used for the treatment of severe malaria or cases where artemisinin-based therapies are not available or not suitable. They are often used in combination with other antimalarial drugs for maximum efficacy.
Atovaquone-Proguanil: This combination is used for the treatment of uncomplicated malaria caused by chloroquine-resistant Plasmodium falciparum or other species. Atovaquone-proguanil is also used for malaria prevention in travelers to malaria-endemic areas.
Primaquine: Primaquine is an antimalarial drug used for the treatment of Plasmodium vivax or Plasmodium ovale malaria to prevent relapse by targeting dormant liver stages (hypnozoites). It is typically used in combination with other antimalarial drugs.
Diagnosis
Clinical Assessment: Healthcare providers evaluate the patient’s symptoms, medical history, travel history (if applicable), and physical examination findings. While clinical assessment alone is not sufficient for a definitive diagnosis, it can help guide the need for further testing.
Microscopic Examination of Blood Smears: This is the gold standard for malaria diagnosis. A blood sample is obtained from a finger prick or venous blood draw, and a thin blood smear is prepared and stained with Giemsa or other suitable stains. The stained smear is then examined under a microscope to detect the presence of malaria parasites (Plasmodium species), as well as the parasite’s stage of development.

Rapid Diagnostic Tests (RDTs): RDTs are simple, point-of-care tests that detect specific antigens produced by malaria parasites in a patient’s blood sample. RDTs are easy to use, require minimal training, and provide rapid results within 15-20 minutes. They are particularly useful in settings where microscopy is not available or feasible.
Molecular Methods (PCR): Polymerase Chain Reaction (PCR) assays can detect and identify malaria parasites by amplifying and analyzing their genetic material (DNA or RNA). PCR assays are highly sensitive and specific, capable of detecting low levels of parasites and identifying the species of Plasmodium present. However, PCR testing requires specialized laboratory equipment and trained personnel, limiting its availability in resource-limited settings.
Serological Tests: Serological tests detect antibodies produced by the immune system in response to malaria infection. While serological tests can indicate previous exposure to malaria parasites, they are not suitable for diagnosing acute infections because antibodies may persist in the bloodstream long after the infection has been cleared.

FAQ (frequently asked questions)
Q. What is malaria? Ans. Malaria is a life-threatening disease caused by parasites of the Plasmodium genus. It is transmitted to humans through the bites of infected female Anopheles mosquitoes.
Q. What are the symptoms of malaria? Ans. Common symptoms of malaria include fever, chills, sweating, headache, muscle aches, fatigue, nausea, and vomiting. In severe cases, it can lead to complications such as organ failure and death.
Q. Where is malaria found? Ans. Malaria is prevalent in tropical and subtropical regions, particularly in Africa, Southeast Asia, and South America. It is a significant public health problem in many countries with limited resources.
Q. How is malaria diagnosed? Ans. Malaria is diagnosed through a combination of clinical assessment and laboratory tests. Common diagnostic methods include microscopic examination of blood smears, rapid diagnostic tests (RDTs), and molecular methods such as PCR assays.
Q. How is malaria treated? Ans. Malaria is treated with antimalarial medications, which vary depending on factors such as the species of Plasmodium causing the infection and the severity of the illness. Artemisinin-based combination therapies (ACTs) are the recommended first-line treatment for uncomplicated malaria caused by Plasmodium falciparum.
Q. How can malaria be prevented? Ans. Preventive measures for malaria include the use of insecticide-treated bed nets, indoor residual spraying, mosquito control measures, personal protection measures (e.g., wearing long-sleeved clothing, using insect repellents), chemoprophylaxis for travelers, and community education.
Q.Is there a vaccine for malaria? Ans. Yes, a malaria vaccine called RTS,S/AS01 (brand name Mosquirix) has been developed and is approved for use in some countries. However, it is not 100% effective and is primarily recommended for children living in malaria-endemic areas.
Q. Why is malaria a concern? Ans. Malaria is a major public health concern due to its significant morbidity and mortality, particularly in children under five years old and pregnant women. It also imposes a substantial economic burden on affected countries and hinders socio-economic development.
Q. How can I protect myself from malaria when traveling to endemic areas? Ans. Travelers to malaria-endemic areas should take preventive measures such as taking antimalarial medications as prescribed, using insect repellents, sleeping under insecticide-treated bed nets, and avoiding outdoor activities during peak mosquito activity times.
Q. When is world malaria day? Ans. 25 April
Q. Test for malaria? Ans. The most common tests for malaria include microscopic examination of blood smears, rapid diagnostic tests (RDTs), and molecular methods such as PCR assays.
Conclusion
Malaria remains a formidable global health challenge, exacting a heavy toll on human lives and socioeconomic development. However, with sustained political commitment, innovative approaches, and multisectoral collaboration, malaria elimination is within reach. By building on past successes and redoubling our efforts, we can turn the tide against this ancient scourge and create a healthier, more prosperous world for all.
Table of Contents
Read more about Malaria
Go and visit dusearchit.in and get more knowledge about others topics.

Pingback: Typhoid-deadly disease-causes, symptoms..(2024)