What is Dengue Fever?
Dengue fever is caused by the dengue virus, which is transmitted to humans primarily by Aedes mosquitoes, particularly Aedes aegypti and Aedes albopictus. The virus exists in four distinct serotypes (DEN-1, DEN-2, DEN-3, and DEN-4), and infection with one serotype does not provide immunity against the others. The disease manifests in a spectrum ranging from mild flu-like symptoms to severe dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS), which can be life-threatening.
The history of dengue is quite extensive and reflects its significance as a global health issue. Here’s a brief overview:
History of dengue fever
Ancient Records and Early Observations
- Ancient Times: Dengue-like illnesses were documented in various ancient texts, including Chinese medical writings from the 5th century AD, which describe symptoms resembling dengue fever.
- 18th Century: The term “dengue” itself is believed to come from the Swahili word “dengue,” which means “cramp” or “pain,” reflecting the disease’s painful symptoms. The first documented outbreak of dengue fever was recorded in the Caribbean in the early 18th century.
19th and Early 20th Centuries
- 1906: The term “dengue” was officially used when an outbreak occurred in the Philippines. The disease was identified as a distinct clinical entity from other febrile illnesses.
- 1950s-1960s: During this period, the link between dengue and the Aedes aegypti mosquito was firmly established. The discovery of the dengue virus and the identification of its four distinct serotypes (DEN-1, DEN-2, DEN-3, and DEN-4) were significant milestones. The term “dengue hemorrhagic fever” was also introduced to describe severe forms of the disease.
Modern Era
- 1970s: Dengue fever began to spread more widely, partly due to increased global travel and urbanization. The World Health Organization (WHO) recognized dengue as a major international public health concern.
- 1990s-2000s: The emergence of dengue epidemics in various parts of the world, including the Americas and Southeast Asia, highlighted the growing problem of the disease. The term “dengue hemorrhagic fever” was increasingly used to describe severe cases, and efforts to control the disease intensified.
- 2010s-Present: There has been a significant increase in the incidence of dengue globally. The WHO has classified dengue as a major global health threat, and there have been efforts to develop vaccines and improve vector control measures. The introduction of the first dengue vaccine, Dengvaxia, in some countries represented a significant step forward, although it has been accompanied by debates regarding its safety and efficacy.
Causes of dengue fever
Dengue is caused by the dengue virus, which is transmitted to humans through the bites of infected mosquitoes. Here’s a detailed look at the causes and factors contributing to dengue:

1. Dengue Virus
- Four Serotypes: There are four distinct but closely related viruses (serotypes) that cause dengue: DEN-1, DEN-2, DEN-3, and DEN-4. Infection with one serotype provides immunity only to that specific serotype. Subsequent infections with different serotypes can increase the risk of severe forms of the disease.
- Virus Transmission: The dengue virus is an RNA virus belonging to the Flavivirus genus. It primarily infects humans but can also infect other primates.
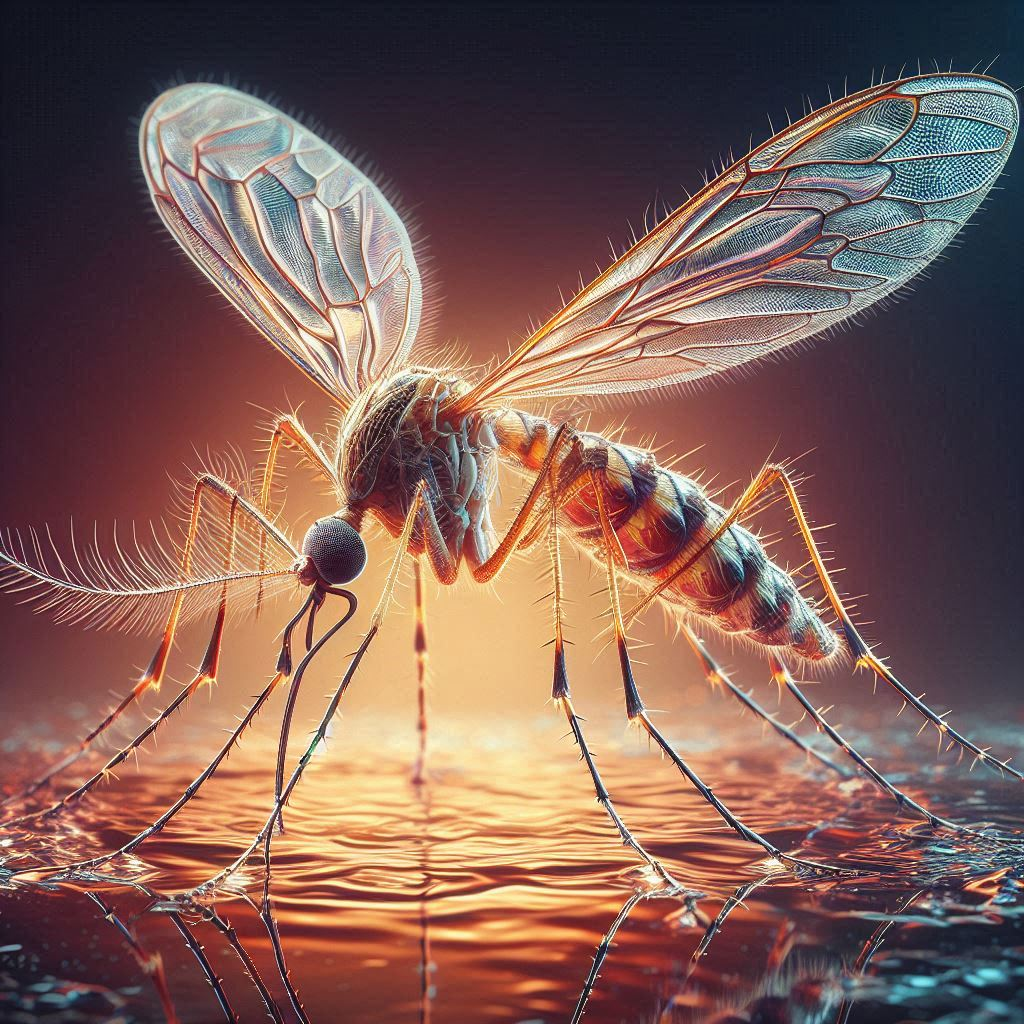
2. Mosquito Vectors
- Primary Vectors: The main vectors are mosquitoes of the species Aedes aegypti and, to a lesser extent, Aedes albopictus. These mosquitoes are characterized by their white markings on the legs and a lyre-shaped pattern on the thorax.
- Transmission Process: The mosquitoes become infected with the dengue virus when they bite a person who is already infected. The virus then replicates within the mosquito, and when it bites another person, it transmits the virus through its saliva.
3. Environmental and Social Factors
- Climate: Dengue is prevalent in tropical and subtropical regions where the climate supports mosquito breeding. Warm temperatures and high humidity are conducive to mosquito survival and reproduction.
- Urbanization: Rapid urbanization and inadequate infrastructure, such as poor sanitation and water management, create breeding grounds for mosquitoes. Stagnant water in containers, discarded tires, and other receptacles can harbor mosquito larvae.
- Global Travel: Increased international travel contributes to the spread of dengue. Travelers can bring the virus to new areas, leading to outbreaks in regions previously unaffected.
4. Human Factors
- Population Density: High population density in urban areas increases the likelihood of mosquito-human contact and facilitates the spread of the virus.
- Immunity: Individuals who have been previously infected with one serotype are at increased risk of severe dengue if they are later infected with a different serotype. The term “antibody-dependent enhancement” (ADE) describes this phenomena.
5. Genetic Factors
- Host Susceptibility: Genetic factors may influence an individual’s susceptibility to severe forms of dengue. Some people might be more prone to severe disease due to genetic variations in immune response.
Prevention and Control Measures
Efforts to prevent and control dengue focus on reducing mosquito populations and minimizing human exposure to mosquito bites. This includes:
- Eliminating Breeding Sites: Regularly removing standing water where mosquitoes can breed.
- Using Mosquito Repellents: using insect repellents with DEET, picaridin, or lemon eucalyptus oil in them.
- Wearing Protective Clothing: Wearing long-sleeved shirts and long pants to reduce skin exposure.
- Implementing Vector Control Programs: Community-wide initiatives to control mosquito populations, including the use of insecticides and biological control agents.
Symptoms of dengue fever
Dengue symptoms can vary widely from mild to severe and typically appear 4 to 10 days after being bitten by an infected mosquito. Here’s a breakdown of the symptoms:
Mild Dengue Fever
- Fever: Sudden high fever, often reaching up to 104°F (40°C).
- Headache: Severe headache, often concentrated behind the eyes.
- Pain: Intense joint and muscle pain, sometimes referred to as “breakbone fever” due to the severity.
- Rash: Skin rash that can appear a few days after the fever starts.
- Nausea and Vomiting: Feelings of nausea and occasional vomiting.
- Fatigue and Weakness: General fatigue and weakness can persist even after the fever subsides.
- Loss of Appetite: Reduced appetite or nausea.

Severe Dengue (Dengue Hemorrhagic Fever or Dengue Shock Syndrome)
Severe dengue can develop from mild dengue and usually manifests in the critical phase of the illness. Symptoms of severe dengue include:
- Bleeding Symptoms:
- Gum Bleeding: Bleeding from the gums.
- Nosebleeds: Frequent nosebleeds.
- Skin Bleeding: Easy bruising and small blood spots under the skin (petechiae).
- Fluid Leakage:
- Abdominal Pain: Severe abdominal pain or tenderness due to fluid leakage into the abdominal cavity.
- Ascites: fluid build-up within the abdominal cavity.
- Pleural Effusion: Fluid accumulation in the chest cavity, which can cause difficulty in breathing.
- Shock:
- Rapid Drop in Blood Pressure: Leading to dengue shock syndrome (DSS), characterized by a significant drop in blood pressure, causing symptoms like dizziness, confusion, and fainting.
- Weak, Rapid Pulse: Indicative of cardiovascular shock.
- Organ Dysfunction:
- Liver Damage: Elevated liver enzymes and signs of liver dysfunction.
- Kidney Dysfunction: Impaired kidney function in severe cases.
Recovery Phase
After the critical phase, most people with dengue fever recover within a few days. However, the recovery phase may be characterized by:
- Fatigue: Prolonged fatigue and weakness.
- Mood Changes: Mood swings and irritability.
Warning Signs for Severe Dengue
Early detection and proper medical care are crucial. If symptoms progress to include any signs of severe dengue, it’s important to seek medical attention immediately. The warning signs include:
- Persistent abdominal pain.
- Vomiting (especially if persistent or with blood).
- Rapid breathing or difficulty breathing.
- Bleeding gums or nosebleeds.
- Extreme fatigue or restlessness.
- Blood in vomit or stool.
Transmission of dengue fever
Dengue is transmitted primarily through the bites of infected mosquitoes. Here’s a thorough examination of the transmission procedure:
Primary Transmission Pathway
- Mosquito Vectors:
- Aedes aegypti: The primary mosquito vector responsible for the transmission of dengue virus. It is recognized by its white markings on its legs and a lyre-shaped pattern on its thorax.
- Aedes albopictus: Also known as the Asian tiger mosquito, it can transmit dengue but is less common than Aedes aegypti.
- Infection Cycle:
- Virus in Mosquitoes: The dengue virus enters a mosquito when it feeds on the blood of an infected person. The virus then replicates within the mosquito.
- Mosquito Transmission: Once infected, the mosquito can transmit the virus to other humans through its saliva when it bites to feed. The mosquito injects the virus into the bloodstream of the new host.
Human-to-Mosquito Transmission
- Infected Humans: People with dengue fever, particularly during the febrile phase (when fever is present), are the primary source of the virus for mosquitoes. They can transmit the virus to mosquitoes that bite them.
- Mosquito-to-Human Transmission: Infected mosquitoes then spread the virus to other humans, continuing the transmission cycle.
Transmission Dynamics
- Geographic Distribution:
- Tropical and Subtropical Regions: Dengue is primarily found in tropical and subtropical regions of the world. The virus is prevalent in Southeast Asia, the Western Pacific, the Americas, and Africa.
- Urban and Peri-Urban Areas: Aedes mosquitoes thrive in urban and peri-urban environments where there are abundant breeding sites, such as in and around human dwellings.
- Breeding Sites:
- Stagnant Water: Aedes mosquitoes lay their eggs in stagnant water. Common breeding sites include water-filled containers, tires, flower pots, buckets, and any other items that can hold water.
- Urban Environments: Poor sanitation, unregulated water storage, and inadequate waste management contribute to the proliferation of mosquito breeding sites.
Secondary Transmission Routes
- Intrauterine Transmission:
- Pregnancy: There is evidence that dengue virus can be transmitted from a mother to her baby during pregnancy, though this is less common. Infants born to infected mothers can have dengue virus detected in their blood shortly after birth.
- Blood Transfusion and Organ Transplantation:
- Rare Transmission: While rare, dengue virus can be transmitted through blood transfusions and organ transplants if the donor is infected.
Not Transmitted By
- Direct Contact: Dengue is not transmitted through direct human-to-human contact, such as touching or kissing.
- Airborne Transmission: The virus is not spread through the air or through respiratory droplets like the flu or cold viruses.
Prevention Measures
To reduce the risk of dengue transmission, several measures can be taken:
- Mosquito Control: Eliminate or manage breeding sites by removing stagnant water and using mosquito larvicides.
- Personal Protection: Use insect repellents, wear long-sleeved clothing, and use mosquito nets or screens to reduce exposure to mosquito bites.
- Community Efforts: Engage in community-wide vector control programs and public education campaigns to reduce mosquito populations and awareness about dengue prevention.
Preventions of dengue fever
Preventing dengue primarily involves reducing mosquito exposure and controlling mosquito populations. Here’s a comprehensive approach to prevention:
1. Personal Protection
- Use Mosquito Repellents: Apply insect repellents that contain DEET, picaridin, oil of lemon eucalyptus, or IR3535. Comply with the manufacturer’s guidelines to ensure safe and efficient operation.
- Wear Protective Clothing: To reduce skin exposure, wear long sleeves, long pants, socks, and shoes. Wearing light-colored clothing is better since dark hues draw insects.
- Use Mosquito Nets and Screens: Sleep under mosquito nets, especially in areas where dengue is common. Make sure there are screens on windows and doors to keep mosquitoes out.
2. Mosquito Control
- Eliminate Breeding Sites: Regularly remove standing water from containers such as buckets, flower pots, old tires, and other items where mosquitoes can breed. Empty and clean water containers weekly.
- Use Larvicides: Apply larvicides to water storage containers that cannot be emptied to kill mosquito larvae. Common larvicides include temephos and biological agents like Bti (Bacillus thuringiensis israelensis).
- Maintain Clean Environments: Keep areas around homes and communities clean and free from trash that can collect water and serve as mosquito breeding sites.
3. Community and Environmental Measures
- Community Clean-Up Drives: Participate in or organize community clean-up efforts to remove potential mosquito breeding sites and promote public awareness.
- Public Health Campaigns: Support and engage in public health campaigns that educate communities about dengue prevention and the importance of mosquito control.
- Vector Control Programs: Support local vector control initiatives that may involve spraying insecticides, using biological control agents, or other measures to reduce mosquito populations.
4. Travel Precautions
- Travel Advisory: If traveling to regions where dengue is common, take extra precautions to avoid mosquito bites, especially during peak mosquito activity periods (dawn and dusk).
- Stay in Air-Conditioned or Screened Rooms: Stay in accommodations with air conditioning or screens on windows and doors to reduce mosquito exposure.
5. Monitoring and Surveillance
- Health Monitoring: Be aware of dengue symptoms, especially if traveling to or living in areas where the disease is prevalent. For the condition to be managed, early detection and treatment are essential.
- Report Cases: Report any suspected cases of dengue to local health authorities to assist in monitoring and controlling outbreaks.
6. Vaccination
- Dengue Vaccine: In some regions, a vaccine called Dengvaxia is available. It’s recommended for individuals aged 9-45 who have had a prior dengue infection. The vaccine is not suitable for those who have never been infected with dengue, as it may increase the risk of severe dengue in subsequent infections.
Diagnosis and treatment of dengue fever
Diagnosis of Dengue fever
1. Clinical Evaluation
- Medical History: Includes recent travel to dengue-endemic areas, mosquito exposure, and symptom onset.
- Physical Examination: Assessment for fever, rash, joint and muscle pain, bleeding signs, and fluid accumulation.
2. Laboratory Tests
- Serological Tests:
- Dengue NS1 Antigen Test: Detects the dengue virus’s non-structural protein 1 (NS1) in the blood, most effective in the early stages (first 5 days of fever).
- Dengue IgM and IgG Antibody Tests: Identify antibodies against the dengue virus. IgM indicates recent infection, while IgG suggests past or secondary infection.
- Molecular Tests:
- Polymerase Chain Reaction (PCR): Detects dengue virus RNA in the blood, confirming the presence of the virus, especially useful in the early phase of illness (first 7 days).
- Hematological Tests:
- Complete Blood Count (CBC): Checks for low white blood cells (leukopenia) and platelets (thrombocytopenia). Elevated hematocrit levels may indicate plasma leakage.
- Liver Function Tests: May show elevated liver enzymes in severe cases.
3. Differential Diagnosis
- Chikungunya Virus: Similar symptoms but with more joint pain.
- Zika Virus: Can present with rash and joint pain.
- Leptospirosis: Bacterial infection with fever and rash.
- Typhoid Fever: Prolonged fever and gastrointestinal symptoms.
- Malaria: Parasitic infection with fever, but different treatment.
Treatment of Dengue fever
1. Supportive Care
- Hydration: Maintain adequate fluid intake to prevent dehydration and manage symptoms. Oral rehydration solutions (ORS) or intravenous fluids may be necessary, especially if there are signs of fluid leakage or shock.
- Pain and Fever Management: Use acetaminophen (paracetamol) to manage fever and pain. Avoid non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or aspirin, as they can increase bleeding risk.
- Rest: Make sure you get enough sleep so your body can heal.
2. Monitoring
- Regular Monitoring: Monitor for signs of severe dengue, such as bleeding, abdominal pain, fluid accumulation, and signs of shock. Regular check-ups and laboratory tests may be required to track the patient’s condition.
- Hospitalization: Severe cases or patients at risk of severe dengue may need hospitalization for close monitoring and management.
3. Specific Interventions
- Blood Transfusion: May be required if there is severe bleeding or significant drop in platelet count.
- Intravenous Fluids: Administered to manage fluid balance, especially if there is evidence of plasma leakage or shock.
4. Severe Dengue Management
- Severe Dengue (Dengue Hemorrhagic Fever and Dengue Shock Syndrome): Requires intensive medical care, including intravenous fluid management, blood transfusions, and close monitoring for complications.
5. Preventive Measures
- Avoid Mosquito Bites: Continue using repellents, wearing protective clothing, and using mosquito nets.
- Vaccination: Dengvaxia is available in some regions for individuals who have had a previous dengue infection. It is not recommended for those without prior dengue exposure due to the risk of severe dengue.
6. Home Care
- Rest and Hydration: Emphasize the importance of rest and adequate fluid intake. Avoid self-medicating with painkillers not recommended for dengue.
- Seek Medical Attention: If symptoms worsen or there are signs of severe dengue, seek medical attention promptly.

Frequently Asked Questions(FAQ’s)
1. What is dengue fever?
Dengue fever is a viral illness caused by the dengue virus, transmitted by mosquitoes, primarily Aedes aegypti. It causes symptoms ranging from mild fever to severe, life-threatening conditions.
2. How is dengue transmitted?
Dengue is transmitted through the bites of infected Aedes mosquitoes. The mosquitoes acquire the virus from biting a person who is already infected with dengue and then spread it to other humans through subsequent bites.
3. What are the symptoms of dengue fever?
Symptoms of dengue fever can vary from mild to severe and include:
- High fever
- Severe headache
- Pain behind the eyes
- Joint and muscle pain
- Nausea and vomiting
- Rash
- Fatigue
Severe cases may present with bleeding, fluid leakage, and organ failure.
4. How is dengue diagnosed?
Dengue is diagnosed through:
- Clinical Evaluation: going over the physical examination, medical history, and symptoms.
- Laboratory Tests: Including Dengue NS1 antigen test, Dengue IgM and IgG antibody tests, and PCR for dengue virus RNA. Hematological tests may show changes in blood counts.
5. What is the treatment for dengue?
There is no specific antiviral treatment for dengue. Management focuses on:
- Supportive Care: Hydration, pain and fever management with acetaminophen (paracetamol), and rest.
- Monitoring: Regular monitoring for severe symptoms and potential complications.
- Hospitalization: Required for severe cases to manage fluids, blood transfusions, and intensive care if necessary.
6. How can dengue be prevented?
Prevention strategies include:
- Reducing Mosquito Exposure: Use repellents, wear protective clothing, and use mosquito nets.
- Controlling Mosquito Breeding Sites: Eliminate standing water in containers and use larvicides.
- Community Efforts: Engage in community clean-up and mosquito control programs.
- Travel Precautions: Take extra precautions if traveling to dengue-endemic areas.
7. Is there a vaccine for dengue?
Yes, Dengvaxia is a vaccine available in some regions for individuals aged 9-45 who have had a prior dengue infection. It is not recommended for those without previous dengue exposure due to the risk of severe dengue in subsequent infections.
8. Can dengue fever be spread from person to person?
No, dengue is not spread through direct contact between people or through respiratory droplets. It is spread only through mosquito bites.
9. What are the warning signs of severe dengue?
Warning signs of severe dengue fever include:
- Severe abdominal pain
- Persistent vomiting
- Bleeding gums or nosebleeds
- Rapid breathing or difficulty breathing
- Extreme fatigue or restlessness
- Blood in vomit or stool
10. How long does dengue fever last?
Dengue fever typically lasts about 1-2 weeks. The acute phase of fever usually lasts 2-7 days, followed by a recovery period. Severe forms may require longer recovery and medical intervention.
11. Can dengue be treated at home?
Mild cases of dengue can be managed at home with proper hydration, rest, and fever management with acetaminophen. However, severe cases or those showing warning signs should seek medical attention immediately.
12. How do I know if I need to see a doctor for dengue fever?
If you experience symptoms of dengue and have been in an area where the disease is prevalent, it is important to see a doctor. Seek immediate medical attention if you develop severe symptoms or warning signs of severe dengue.
13. Is dengue common in my area?
Dengue is common in tropical and subtropical regions. Check with local health authorities or travel advisories for information on the prevalence of dengue in specific areas.
14. Can dengue affect children and pregnant women?
Yes, dengue can affect people of all ages, including children and pregnant women. Special care and monitoring are required for these groups, especially if symptoms are severe or complications arise.
Conclusion
Dengue fever remains a major public health challenge in many parts of the world, with significant implications for affected individuals and communities. Awareness, prevention, and prompt management are crucial in controlling the spread of the disease and reducing its impact. By understanding the causes, symptoms, and preventive measures, individuals and communities can better protect themselves against this potentially severe illness.
Table of Contents
Read more about Dengue
Go and visit dusearchit.in and get more knowledge about others topics.
